Background and Context
The Fair Work Agenda in Scotland
As Scotland’s Fair Work Framework[2] highlights, work is crucial to the prosperity, health and wellbeing of most people and every society. What happens at work and the characteristics of work are of huge significance to individuals and policy makers. Both the quantity of work and its quality are increasingly recognised in national and international debates and policy.
Scotland’s employment statistics – the numbers of people in employment and those unemployed – have improved significantly over recent years. There are, however, concerns over the quality of work and employment. This includes rising levels of economic inactivity, disparity in access to jobs and the rise of more flexible, but less secure forms of work such as zero hours contracts, temporary work and so called ‘sham’ self-employment. For a significant minority of people, the labour market is not delivering the decent wages or stability they need and there are a number of structural factors which negatively impact peoples’ actual experience of work, such as power imbalances in the work place and lack of representation and voice, lack of investment in training and general job insecurity.[3]
The impacts of bad jobs are most evident for individual workers; if a person has a poor-quality job they are more likely to live in poverty, in working life and beyond, their children are more likely to live in poverty, and their chances of accessing training or development are lower. However, it is not just workers in bad jobs that lose out, employers also miss out on the benefits that good work brings: more engaged, committed and adaptable workers who identify challenges, solve problems and are able to offer insight and ideas for business or service improvement. At the level of the economy too, fair work matters; many of the practices associated with high quality work are more prevalent in societies with higher productivity and higher rates of business and service innovation than Scotland or the UK.[4] Unfortunately, however, Scotland’s economy is made up of too many poor jobs with poor working conditions, which undermine peoples’ potential and sustain inequality.
Scotland’s aspiration is to be a leading fair work nation. Fair work means that workers are paid and treated fairly, with opportunities to progress, learn and have a voice on what matters to them. It includes fair pay, safe and healthy workplaces, respectful treatment, sufficient hours, opportunities to progress and access to effective voice mechanisms to deal with problems and conflicts, but also to ensure a channel through which to communicate and influence.
The growing importance of fair work is recognised by the Scottish Government. It is central to Scotland’s Economic Strategy and is underpinned by measurable indicators in the National Performance Framework. While some levers to influence fair work are not available to Scotland (such as employment law powers), government has other ways of influencing practice through policy, procurement, leadership and investment in fair work infrastructure that can drive change. Scotland’s approach to fair work illustrates the range of areas that need to be addressed to enhance work and employment quality, well-being, labour market and economic outcomes.
Why has the FWC prioritised Social Care?
The role of the Fair Work Convention is to advise Scottish Government on fair work and to advocate for fair work in Scotland, creating benefits for individuals and their families, businesses and society. Challenges in delivering the various dimensions of fair work differ across firms and sectors. The social care sector is often depicted as being a sector in crisis as a result of rising demand, severe funding pressures and high staff turnover. People are waiting longer than previously for services and unpaid care is filling some of the gaps. It is well documented that care work is low-paid, female-dominated and undervalued, with pay rates in the voluntary and private sector close to the minimum wage despite the complexity of the roles and the skills and qualifications required. There have been many reports about care providers struggling financially, with examples of contracts being handed back and services closing.[5] The sector is also finding it difficult to recruit and retain its workforce and concerns are growing that vital employees from the European Union are leaving the workforce due to Brexit.[6]
The Social Care Sector in Scotland
The social care sector employs 7.7% of the Scottish labour force, and is a diversified market in terms of provision (See Figure 1).
Figure 1: Social care workforce by employer type, 2017
Source: Scottish Social Service Council, 2017
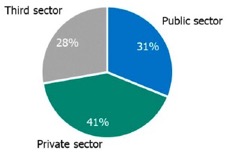
Figure 2: Scottish Social Services Workforce Data
Source: Scottish Social Services Council, 2008 – 2017 data
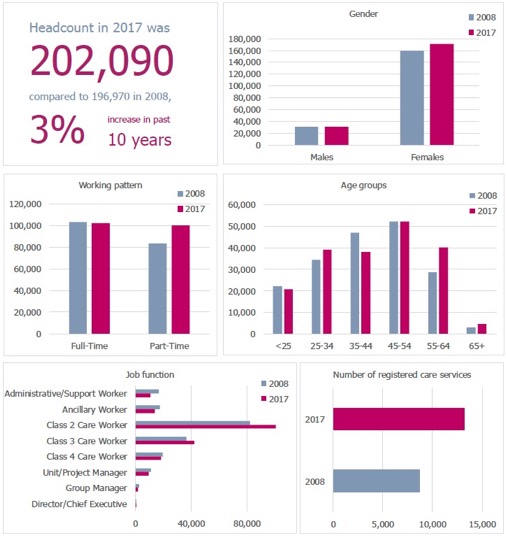
Note: ‘Don’t know’ responses were excluded
The 2008 data on gender, working pattern, age and job function does not include figures for the number of childminders in work
Context and Recurring Themes
Scotland has a number of strategies for reforming and improving care services to meet changing patterns of need and to face a cost-constrained environment. This includes work to develop an integrated health and social care system to plan accordingly for its workforce. Many interventions are about redesigning the system towards a more outcomes - and human rights - focused agenda, driven by the desire to support older people, disabled people and other service users to participate actively in their communities and to lead good lives, such as Self-Directed Support and developing innovative neighbourhood-based models of care. Policy continues to support the development of care standards and qualification requirements alongside payment of the Living Wage for care workers. Most recently, the Scottish Government and COSLA has begun to discuss reforming adult social care.[7]
In this broad policy context, the following themes came up repeatedly during discussions of the Social Care Working Group (see Appendix B for membership) when reflecting on the fair work experiences of the social care workforce:
- The undervaluing of social care work
- Gender and undervaluation and the lack of voice and visibility of this workforce
- Health and social care disparities: how the care sector is treated relative to the health sector and the differences with how the workforces are treated and supported
- Personalisation, Self-Directed Support and the balance between the rights of users and the rights of workers
- Accessing training in an increasingly professionalised service
- Challenges from downward pressures on funding and budgets
- Recruitment and retention challenges
- Low pay in the sector and issues around Living Wage implementation
- Commissioning practices and the ongoing legacy of the purchaser-provider split.
The undervaluing of social care work
“There isn’t enough money and that’s a lot to do with the value of the profession, the way the profession is considered by society”.[8]
Frontline workers feel respected for the work they do by their colleagues, those they care for and their employers, but they do not feel particularly valued by Scottish Government or the wider public.[9] Many stakeholders perceived the dominant narrative in Scotland as focusing on the importance of the NHS and health. Social care, although an important service, was perceived as a poor relation in wider policy and political debates, with perceptions of widespread under-appreciation of social care by the public, particularly when compared to Health. Social care employees' terms and of conditions fall short of their counterparts in the health sector. Yet as the health and social care integration agenda recognises, social care is important to society and to the economy, affecting the lives and life chances of people needing care and support, their families, the social care workforce, care providers and the NHS. Social care is important to health prevention, citizens’ well-being and social inclusion. The social care sector provides 200,000 jobs and contributes over £4 billion to the economy.[10] The sector plays an important role in initial training and skills development for thousands new to employment every year and, is becoming increasingly qualified and professional. It is a particularly important labour market for women, especially older women, as women in their later working lives move into social care employment, providing an important avenue for women’s economic empowerment and security.
Gender and under-valuation
The evidence suggests that the undervaluing of care work is, to a significant extent, linked to the predominance of women workers in the sector.[11] The view of the Social Care Working Group was that part of the failure to value social care comprehensively is due to its status as women’s work (see Figure 2). Women face systematic labour market disadvantage, including occupational segregation, workplace discrimination and lack of flexible working. Institutionalised undervaluation is common in highly feminised jobs and occupations, contributing to the gender pay gap (of 15% in Scotland). Social care work is also less visible than other work, taking place in service user’s homes rather than workplaces, with implications for skills recognition and for collective organising.
Evidence suggests that care work is rewarding and fulfilling,[12] yet this is not a replacement for pay and other material rewards of work. The choice to engage in care work is not a choice to earn low wages or face variable work patterns. Social care work is often locally based, which is attractive to women who may need to juggle paid work with unpaid care work at home. Addressing how the sector and it workforce is valued is, therefore, important to delivering on the opportunity dimension of fair work.
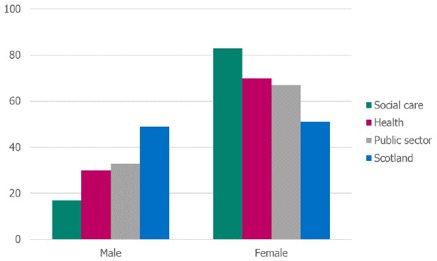
Figure 3: Gender split in the social care sector
Source: Labour Force Survey 2017, ONS
Health and social care disparities
The social care workforce is split across a mixed economy of providers in the public, private/independent and third sectors. Workers in local authority services generally have relatively better terms and conditions.
Notwithstanding moves towards health and social care integration, terms and conditions in social care fall far short of those in comparable jobs in the health sector. Health employees have higher levels of union membership and more powerful professional bodies, while NHS Scotland workers have well developed partnership working and collective bargaining mechanisms. The social care sector lacks crucial infrastructure vital for the comprehensive embedding and delivery of fair work outcomes for workers. Union penetration in this sector is limited. Due to the nature of the work – not in conventional workplaces - social care is a challenging environment for unions to operate in and for workers to engage collectively. This undermines effective employee voice, and the fragmented nature of the sector exacerbates this problem. This includes voice mechanisms which would allow the workforce to engage collectively and negotiate better terms and conditions.

Source: Labour Force Survey 2017, ONS
Yet care is a skilled and increasingly professionalised sector with many features shared with the health sector: workers often dispense medicine and care for people with complex conditions; they provide intense emotional support to those they care for and their families; and they liaise with other health professionals. All social care workers are formally registered with the Scottish Social Services Council (SSSC);[13] qualifications are now a sector norm and broader occupational classifications within the sector reflect the growing complexity of care. However, pay and rewards have not increased in line with the increasing demands of the job.
Personalisation and Self-Directed Support
Workforce issues have also been raised in the context of personalisation and Self-Directed Support (SDS). The policy environment rightly places the user at the heart of service design, but this has led to the design and delivery of services occurring in isolation, with little or no cognisance of the strain this has placed on the system or on workforce capacity to absorb new policy initiatives or respond to user need.
The move to SDS has been transformational for the sector. SDS represents a significant transfer of choice, power and control to the citizen, while at the same time asking more from care workers in terms of their flexibility, skills and experience to provide a more personalised and responsive service. SDS has huge potential for positive change in how jobs and the sector as a whole are organised and designed. However, Audit Scotland has recently said that SDS is not yet embedded as Scotland’s approach to care. Reports from Scottish Care and the Coalition of Care Providers Scotland (CCPS)[14] show that implementation has been challenging,[15] with commissioning processes not changing quick enough and ‘hours of support’ and ‘hourly rates’ continuing to be used to cost services.
This policy agenda has also raised difficult issues on the balance between the rights of users and workers’ rights.[16] In addition, SDS requires considerable workforce flexibility to deliver new and more responsive models of care, but workers find it hard to fulfil the Codes of Practice and access the right training and supervision to meet the new demands being placed on them. This works to restrict the autonomy of the worker to deliver individualised care and reduces much of the creativity and innovation that improves services on the ground.
Accessing training in an increasingly professionalised service
Policy development has supported an increasingly professionalised social care service, with an emphasis on improving its qualifications profile. There are concerns, however, as to whether policy development has fully recognised the potential impacts on the workforce. The Social Care Working Group heard evidence from care providers that many social care staff take up care posts with no formal qualifications and little or no experience. They are then required to undertake mandatory training and to commit to gaining a professional qualification within a specified period of time. There is no national provision and minimal coordination to support this. Often these new recruits are older women.[17] Wider research identifies this group as particularly vulnerable to poverty as a result of state pension changes. Many are returning to the workplace after breaks in working due to raising a family and may be attracted to the possibility of working flexibly around school hours or other commitments, though research suggests that these entrants to the sector tend not to have prior qualifications in social-care.[18] This places a predominantly older, female workforce under huge pressure. Stakeholders reported on the challenges for workers moving to a qualification-focused system, identifying negative impact on older women workers, some of whom were leaving the sector as a result of the pressure to obtain qualifications. With cuts in funding and tighter contracts, employers are finding it challenging to fund this training, so staff are often expected to pay for their training and SSSC registration themselves. The Social Care Working Group concluded that taking into account the data available on the social barriers and obstacles many workers face in terms of access to information and technology, poor prior experience of education/learning and existing poverty and literacy levels challenges, and recognising the range of health conditions the homecare workforce is supporting, this is particularly demanding.[19] Research suggests, however, that workers did speak highly of the training that they did receive but that there were practical challenges in accessing it, preventing them from benefitting from what was on offer.[20]
In health, where training is crucial for health policy and the NHS overall service quality, government takes on a more proactive role in workforce development and planning. This is not the case in social care. Other than setting standards through Codes of Practice and outlining qualification expectations, there is no intervention by the state in the capacity and capability of the workforce and in the provision of training costs to achieve SSSC recognition.
Downward pressure on funding and budgets
The sector faces real and significant challenges. This includes financial pressures, demands due to changing demographics, the push to design services that meet changing patterns of need and responding to government reforms and demands to maintain higher quality and standards of service.
It is widely accepted that the social care sector is facing severe challenges due to austerity. It is also working to meet the needs of an ageing population that is living longer, but with more complex needs. Evidence taken by the social care working group was that 200,000 people receive adult social care services annually, with 100,000 people receiving half of the total health and social care budget: most are accessing many different aspects of the health and social care system.[21] A balance has to be achieved in terms of eligibility, charging and assessment, how to provide flexibility in the system, how to support those providing informal care and how to support people to stay at home with maximum independence for as long as possible. However, with no significant injection of new money, managing change is a growing burden on the sector.
Most significantly, the social care working group learnt that the pressure to contain costs is driving forms of commissioning that, as discussed below, significantly constrain employers in the sector in delivering fair work to their staff.
Recruitment and Retention challenges
Providers are increasingly finding it harder to fill vacancies, and retain staff once they join. They see these as their biggest challenges, raising concerns over the sustainability of the sector. The Care Inspectorate’s recent report found “more than a third of social care services have reported unfilled staff vacancies” in the past 18 months. Currently women workers over fifty years account for forty-five percent of care workers. Although retention and recruitment issues have long been a problem in the sector,[22] providers are also being challenged by Brexit. 12,000 EU nationals work in health and social care in Scotland, representing around 3% of employment in this sector.
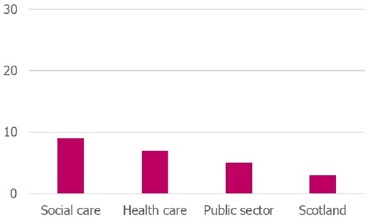
Figure 4: Percentage of social care workers looking for different or additional paid jobs in 2017
Source: Labour Force Survey 2017, ONS
The inability of care providers to attract a workforce relates to pay, terms and conditions and the lack of value placed on a career in social care. Stakeholders perceive that this scenario is driven by current commissioning practices that make jobs less attractive, less secure and less flexible; zero hours contracts, challenges around rota predictability, long hours and requirements to acquire qualifications for registration and unreasonable expectations around availability and overtime.[23] The social care working group heard evidence that contracts are also being affected by budget cuts. This has resulted in decreasing available hours per client, increasing need for part-time contracts to respond to Working Time Directive challenges and night time provision changes. Retrospective cuts and reduced budgets mean that providers are continuously having to look into ‘at risk of redundancy scenarios’. All of this is taking place in circumstances when there is growing demand for social care, and impacts not just on staff experience, but on the attractiveness of the sector to potential recruits. Drawing on the voice and experience of existing care workers to help address some of these challenges in employment and work in the sector may prove to be a significant asset in addressing perceptions of social care and aiding recruitment to the sector.
Low pay and Living Wage implementation
The recent introduction of the Living Wage, while welcome, has faced significant operational challenges causing financial difficulties for providers. Implementation in workplaces has resulted in pay compression with workers in supervisory positions or with greater experience finding themselves paid almost exactly at the same level as new starts.
Although the wage floor has been increased as a result of introducing the Living Wage in care, no mechanism has been devised for undertaking job evaluation and for upgrading the wages for those with greater skills and experience. This has caused difficulties in recruiting and retaining senior posts and managers, with existing workers reluctant to take on additional responsibility for limited financial reward.
Commissioning practices and the ongoing legacy of the purchaser-provider split
Another recurring theme among stakeholders was how the sector as a whole is organised and structured and the problems associated with having a market-led system of tendering. In recent years Scotland Excel has developed more progressive models of Social Care Frameworks, recognised for the Living Wage and fair work ethos, however as described by the organisations providing evidence to this Inquiry, Framework Agreements lead to providers being accepted onto the framework with no agreed level of work. This appears to play a substantial role in passing the risk of adjusting to variable demand onto the provider and subsequently to the worker. This non-committal type of framework arrangement appears to impact directly on the nature and security of employment for a substantial component of the workforce.
Social Care currently operates in a mixed market economy. This was not always the case. Nationally-agreed terms and conditions were once the norm, until legislation in the 1990s[24] opened up market-led provision. Central to the then Conservative Government’s commitment to increasing efficiency through the development of markets was giving local authorities responsibility for assessing needs and commissioning care services, ensuring resources were used effectively, enhancing choice and personalisation and stimulating a mixed economy or a market of care.[25] By 2009, over two thirds of adult social care jobs had moved to the independent sector, with a significant percentage of council provision being delivered by arm’s length bodies. Local authorities were expected to bring budgets under control, which they did by introducing eligibility criteria.
These reforms transformed UK social care practice and provision and caused new problems. As national and local government withdrew from actual service provision, they also withdrew from their role with the workforce (other than for those in the statutory sector who they continued to employ directly), leaving it for the market and providers to manage with little or no support from national government. This has created inequality, not only for workers’ terms and conditions but also in service provision. Local authorities developed different criteria of eligibility, intensified the division between health and social care and weakened the state’s responsibility to the social care worker.[26]
While there are real challenges in how to pay for social care, stakeholders identified an urgent need to address the extent to which the resulting commissioning and contracting system is placing most of the risk and burdens of tight finances and significant policy reform onto the workforce. Both voluntary and private care providers reported downward pressure on budgets as a direct result of procurement processes.
Challenges in commissioning of care services problems identified included:
- Disconnect between strategic planning, service commissioning and procurement approaches
- Failure to provide sufficient resourcing within contracts to allow the delivery of fair work ambitions
- Contracts in which employers struggle to sustain decent pay and conditions (including sick leave and holidays)
- Contracts that do not cover travel costs, especially challenging in rural Scotland
- Difficulties in recruiting and getting existing staff to travel
- High costs of recruiting, particularly in remote areas, where competition is fierce
- Non-funding of management costs
- Growth of split shifts and reductions in paid sleepovers
The market-led system, which creates and relies upon competition has, according to some stakeholders, accelerated a “race to the bottom’ as providers compete to win contracts. Alarmingly, there are examples of online auctioning of contracts which were shared in the Working Group – where providers compete to win contracts at the lowest cost. These types of practices have impacted pay and conditions and undermine fair working practices. Care contracts are often falling short in terms of providing for the full costs of providing fair work.[27] The resulting lack of job security, low pay and expectations of ever-increasing flexibility by workers delivers a workforce at risk of experiencing in-work poverty, inequality and poor health outcomes.
The Scottish Government has acknowledged that workers in the care sector are suffering in the competitive market for care. It is particularly significant that the Scottish Government has felt the need to intervene to correct untenable levels of low pay in the sector by providing additional central funds to pay all social care workers the Living Wage. Whilst welcome, the Living Wage initiative addresses only the hourly rate paid and consequently falls far short of being an effective remedy for the significant structural problems that plague the social care system and act as an impediment to fair work.
Stakeholders agreed that fair work needs to be mainstreamed into social care to turn the tide on recruitment and retention issues in the sector, enhance worker well-being and improve equality. This is inconsistent with procurement contracts which place all the burden of flexibility and adaptation to policy on the care workforce. Some efforts have been made to influence commissioning. The Scottish Government’s statutory procurement guidance (published in 2015) requires all public bodies to have regard to fair work practices in contracts and to abide by best practice Fair Work procurement guidelines. The best practice guidelines and toolkit should be applied at every level – by commissioners and by employers.